November 2022
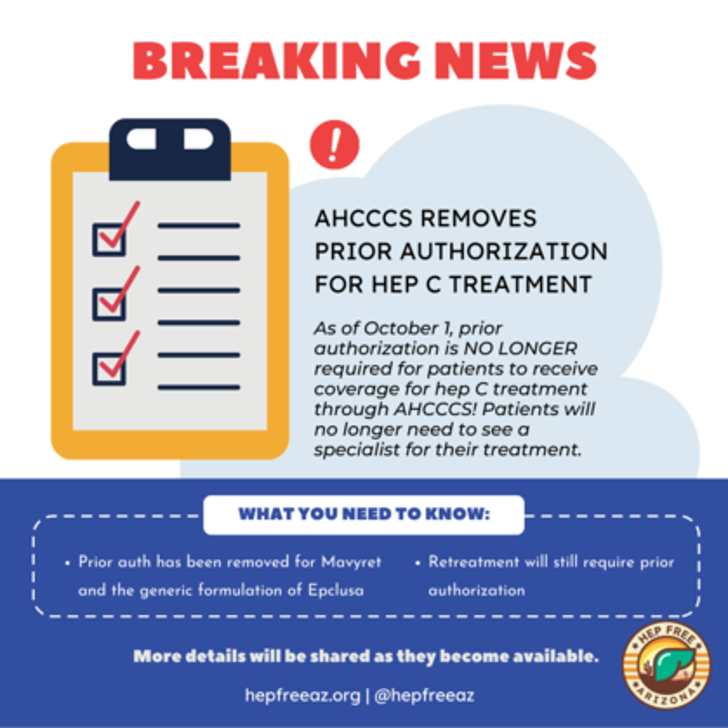
We are thrilled to share that as of October 1, 2022, prior authorization is NO LONGER required for patients to receive coverage for hep C treatment through AHCCCS! Patients will not need to see a specialist for their treatment and providers will no longer need to submit paperwork to be approved for the coverage of Mavyret and the generic formulation of Epclusa. Please note that retreatment will still require prior authorization.
Making Arizona the 16th jurisdiction in the country to remove PAs for hep C treatment, this milestone in our history was truly a patient- and community- led change. Thank you to everyone for the massive contributions and continued advocacy efforts- without you, this would not have happened. Read more on this change here!